SCIENTIFIC ACHIEVEMENT
Researchers have designed a biomedical device for absorbing excess chemotherapy drugs during cancer treatment, characterizing the active surface layer using x-ray microtomography at the Advanced Light Source (ALS).
SIGNIFICANCE AND IMPACT
The work opens up a new route to fighting cancer that minimizes drug toxicity and enables personalized, targeted, high-dose chemotherapy.
Intra-arterial chemotherapy
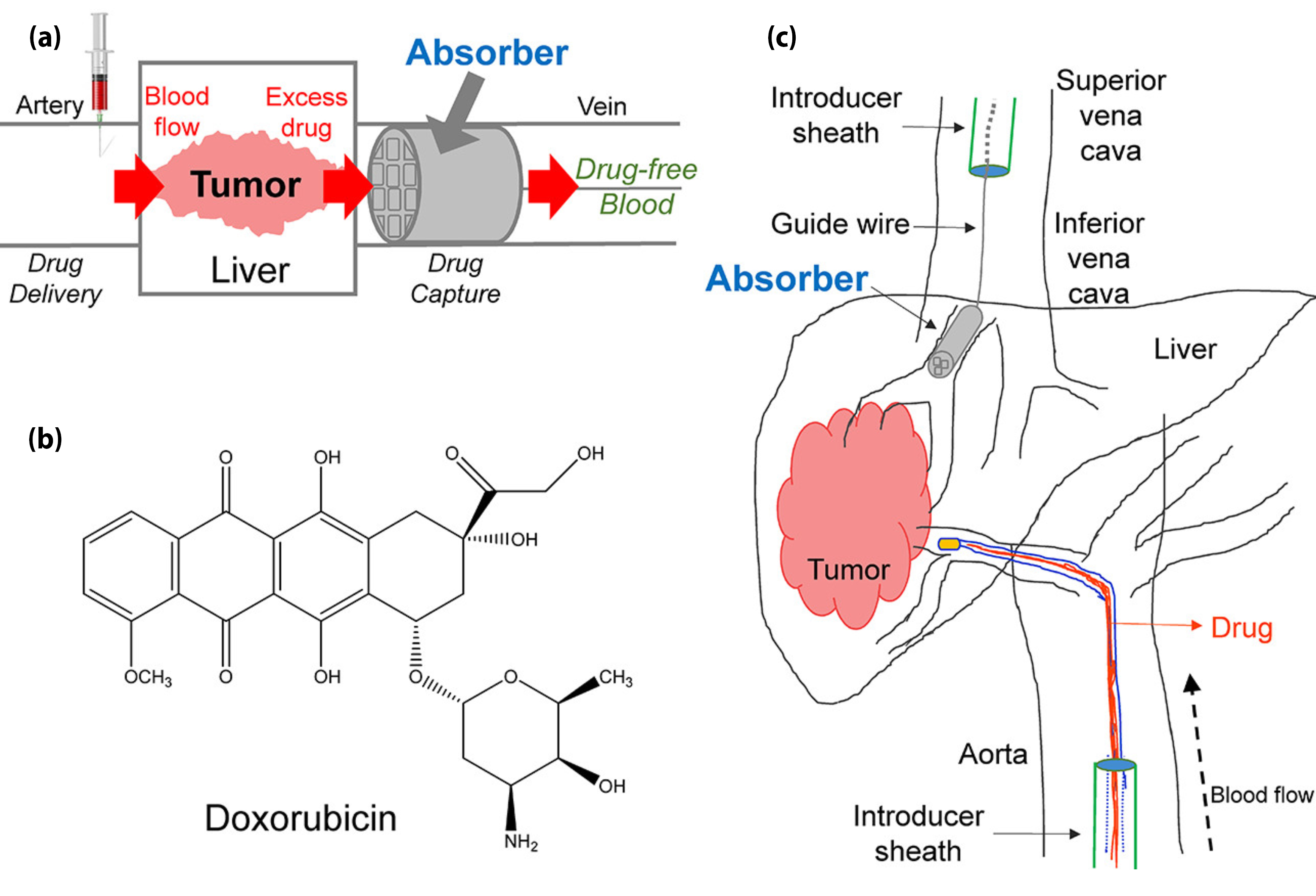
Most anticancer drugs are poisonous, so doctors walk a delicate line when administering chemotherapy. A dose must be sufficient to kill or stop the growth of cancer cells in the target organ, but not high enough to irreparably damage a patient’s other organs. To avoid this, doctors can thread catheters through the bloodstream to deliver chemotherapy drugs directly to the site of the tumor—a method known as intra-arterial chemotherapy. Still, typically more than half of the dose injected into the body escapes the target organ. Several years ago, researchers began working on a major improvement: placing a device “downstream” of the targeted organ to filter out excess chemo so that much less of the drug reaches the body as a whole.
A 3D-printed “drug sponge”
In this work, researchers created “drug sponges,” tiny cylindrical absorbers coated inside with a polymer that has a high affinity for binding doxorubicin, a widely used chemotherapy drug. Designed to be placed in a vein, these devices are 3D printed for each use rather than mass produced, so they can be customized for a given patient. The absorbers tested in these experiments were 5 mm in diameter and 30 mm in length, with an internal support structure of crossbars forming “pores” 800 µm wide. A central hole runs the length of each cylinder to enable attachment of a guide wire needed for minimally invasive surgical placement. After a year’s worth of trial and error, the researchers found a process that appeared to result in a stable, uniform polymer coating throughout the device.
Visualizing the scaffold and coating

To validate the coating method and confirm the uniformity of the coating layer throughout the absorber, the researchers used x-ray microtomography at ALS Beamline 8.3.2. An absorber was first imaged uncoated, then subjected to the coating protocol, and imaged again. The separate tomograms where then superposed, with the coating displayed as a different color. This technique was a critical tool for obtaining a dataset characterizing the entirety of this complex, 3D object without the need to physically slice into it, which could potentially affect the coating’s integrity. The ability to tune the x-ray energy range enabled the researchers to bring out the subtle contrast between the scaffold and the coating—both polymers that would look much the same in other imaging modalities.
Promising early tests and future plans
In preliminary tests in pigs, the researchers found that the absorber bound up, on average, 64% of the doxorubicin injected upstream of a healthy liver. Immediate plans are to see if the scaffolds can be printed with smaller pores, to increase the surface area absorbing the drug molecules without interfering with the flow of blood cells. Human tests are still a few years away, but the researchers envision that this approach could eventually be applied to any drug targeting a particular organ, such as high-powered antibiotics that are required to kill a pathogen. Although much work remains, this study opens a new route to help patients fight disease and improve survival by minimizing drug toxicity.
Contact: Nitash P. Balsara
Researchers: H.J. Oh, M.Y.J. Yi, and W.S. Loo (Univ. of California, Berkeley); M.S. Aboian, M.W. Wilson, T. Moore, C.R. Yee, and S.W. Hetts (Univ. of California, San Francisco); J.A. Maslyn and N.P. Balsara (Univ. of California, Berkeley, and Berkeley Lab); X. Jiang (Berkeley Lab); D.Y. Parkinson (ALS); G.R. Robbins and F.M. Barth (Carbon, Inc.); J.M. DeSimone (Carbon, Inc., Univ. of North Carolina, and North Carolina State Univ.).
Funding: National Instututes of Health; U.S. Department of Energy (DOE), Office of Science, Basic Energy Sciences Program (BES). Operation of the ALS is supported by DOE BES.
Publication: H.J. Oh, M.S. Aboian, M.Y.J. Yi, J.A. Maslyn, W.S. Loo, X. Jiang, D.Y. Parkinson, M.W. Wilson, T. Moore, C.R. Yee, G.R. Robbins, F.M. Barth, J.M. DeSimone, S.W. Hetts, and N.P. Balsara, “3D Printed Absorber for Capturing Chemotherapy Drugs before They Spread through the Body,” ACS Cent. Sci., Article ASAP (2019), doi:10.1021/acscentsci.8b00700.
Adapted from the UC Berkeley news release, “Drug sponge could minimize side effects of cancer treatment.”
ALS SCIENCE HIGHLIGHT #393